While the vaping epidemic seizes U.S. youth, health care professionals can help clear the air by discussing and treating vaping as an addiction.
Based on an article by Novid Parisi from the AMT Pulse, Spring 2020.
Beyond COVID-19, young people face another unprecedented epidemic.
Vaping continues to mount, right alongside hospitalizations and deaths. More than 5 million teenagers are now using e-cigarettes, according to the Food and Drug Administration (FDA). The mystery of just what is happening from vaping is only beginning to be understood.
E-cigarettes, or vapes, come in a variety of styles and shapes. In essence, they are battery-powered devices that heat a nicotine-filled liquid. Puffing the device heats the liquid, which turns into vapor (thus “vaping”) that the user inhales. Just how bad is it to repeatedly pull from the end of a battery? Scientists aren’t fully sure right now. With regular tobacco cigarettes, for instance, it took decades of research to understand the life-threatening effects.
While traditional youth smoking has declined, vaping has skyrocketed—rising 78% among high schoolers and almost 50% among middle schoolers from 2017 to 2018. It’s not just the rampant use that’s worrisome, but the lack of knowledge among users.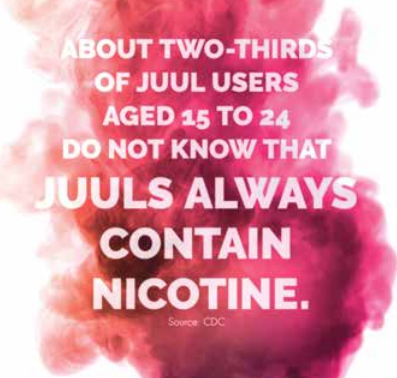
With 27.5% of high schoolers smoking e-cigarettes, healthcare professionals play a potentially lifesaving role in helping to educate users.
Not only is nicotine highly addictive, it’s especially harmful to the adolescent brain, which continues to develop until roughly age 25. Despite marketing claims about “nicotine-free” vaping products, about 99% of commercially sold e-cigarettes contain nicotine, according to the CDC. While e-cigarettes are safer than traditional, combustible cigarettes, that’s an exceptionally low bar when it comes to the health of youth, King says. “Conventional cigarette smoke contains 7,000 chemicals and 70 carcinogens, so most things are safer than that.”
Even vaping products with little nicotine contain a host of other harmful ingredients—toxic metal particles such as nickel and lead, and chemicals such as formaldehyde, acrolein and acetaldehyde—that can cause permanent lung damage. With vaping, these chemicals penetrate the lungs deeply, with some toxic chemicals having the potential to go deeper than traditional cigarettes.
Throught the Smoke
With 84% of Americans seeing a healthcare professional at least once in the previous year, according to the most recent CDC research, healthcare professionals have a special, trusted role to play in combatting the vaping epidemic. Yet many are reluctant to talk about vaping with patients.
 Healthcare professionals often don’t feel comfortable talking about vaping because the products haven’t been around for long, they’re constantly changing and the long-term health effects are not yet known, Vipond says. “It’s hard to know what to talk about.” For starters, though, practitioners should ask patients about both smoking and vaping habits and advise users to quit. But if just telling people to stop was enough, there would be no smokers. “Most smokers know smoking is not good for their health,”
Healthcare professionals often don’t feel comfortable talking about vaping because the products haven’t been around for long, they’re constantly changing and the long-term health effects are not yet known, Vipond says. “It’s hard to know what to talk about.” For starters, though, practitioners should ask patients about both smoking and vaping habits and advise users to quit. But if just telling people to stop was enough, there would be no smokers. “Most smokers know smoking is not good for their health,”
Vipond says. Like traditional smoking, vaping is an addiction, so it should be discussed and treated that way, Galiatsatos says. “Professionals need to know that nicotine addiction is a chronic disease,” he says. They need to apply the same approach they use for other chronic diseases, such as diabetes and hypertension, by asking patients when, how much and why they smoke.
Healthcare professionals also should get informed about vaping terminology and popular brands. Whileclinicians might say things like “electronic nicotine delivery system,” users certainly don’t.
Ultimately, though, there is no ambiguity around the quick rise and effect of e-cigarettes on young people today, Vipond says. “We have a whole new generation of smokers who are getting addicted who would never have considered smoking combustible cigarettes.”
E-Cigarette Resources